 Some children with liver cancer may need less chemotherapy than is typically used to treat the disease, according to results from a phase 3 clinical trial.
Some children with liver cancer may need less chemotherapy than is typically used to treat the disease, according to results from a phase 3 clinical trial.
The study, led by the NCI-supported Children’s Oncology Group, included children and infants with the most common type of childhood liver cancer, hepatoblastoma, whose tumors had been surgically removed when the disease was diagnosed. Such patients subsequently receive chemotherapy to kill any remaining cancer cells.
Liver cancer is rare in children, and only about one-third of these patients have tumors that can be removed surgically at the time of diagnosis.
Approximately 90% of children whose tumors are removed at diagnosis and who receive chemotherapy survive the disease. But some survivors develop lasting side effects of chemotherapy, including hearing loss caused by the drug cisplatin.
Investigators were therefore interested in learning whether a lower dose of chemotherapy could be used to reduce side effects without affecting survival.
In the study, children who received half of the normal amount of chemotherapy survived as long as children who received the full amount in previous trials, researchers reported in The Lancet on April 8.
“We found that four cycles of chemotherapy—the standard amount—were not needed and that two cycles seemed to be enough,” said Howard Katzenstein, M.D., of Nemours Children’s Specialty Care and Wolfson Children’s Hospital in Jacksonville, FL, one of the investigators.
The trial is part of a broader effort by the Children’s Oncology Group and other cancer researchers to evaluate treatment regimens for children with cancerExit Disclaimer that can reduce the risk of side effects without increasing the chances the disease will return.
Focusing on Patients’ Quality of Life
For children with hepatoblastoma who receive “up-front” surgery, it is common to administer chemotherapy in the hospital. In addition to extending the length of a hospital stay, chemotherapy may cause side effects during treatment, such as nausea, vomiting, risk of infection, and kidney damage, Dr. Katzenstein noted.
“In a group of patients with a 90% cure rate, we need to ensure that these children have the best possible quality of life,” said Dr. Katzenstein. The goal of the trial, which also included other patients whose tumors could not be surgically removed at diagnosis, was to “optimize” the amount of adjuvant chemotherapy needed to cure the patients.
In the study, 49 patients with hepatoblastoma who had surgery at diagnosis received two cycles of a combination of three chemotherapy drugs (cisplatin, fluorouracil, and vincristine) rather than the standard four cycles.
After a median follow-up of 42 months, more than 90% of patients in the trial had no symptoms of liver cancer or a recurrence of the disease (an outcome known as event-free survival), the researchers found. This result compares well with the results of previous trials involving surgery plus four cycles of chemotherapy, they noted.
Only one patient in the trial experienced hearing loss. After a median follow-up of 4 years, 95% of the patients were alive; the 5-year overall survival rate was 91%.
“The results of this trial will inform decisions about how the disease is treated in the future,” said Nita Seibel, M.D., head of Pediatric Solid Tumor Therapeutics in NCI’s Cancer Therapy Evaluation Program, who was not involved in the study.
She cautioned, however, that the study was small and that the findings apply only to the care of patients with tumors that surgeons can safely remove at diagnosis. Patients are not candidates for the reduced amount of chemotherapy if their tumors are advanced or have spread to other parts of the body.
“The trial builds on the work of a previous study that reduced the number of cycles of chemotherapy for some patients with hepatoblastoma from six to four,” Dr. Seibel continued. “The ultimate goal of this research is to reduce the amount of chemotherapy a patient needs without compromising outcomes.”
But progress in reaching this goal has been “gradual,” she added, in part because pediatric liver cancer is so rare. Only about 100 to 125 cases of hepatoblastoma are diagnosed in North America each year.
“Hopefully we will get to a point when some of these children may be treated with surgery alone and not receive [any] chemotherapy, but we’re not there yet,” she said.
Guidelines for Selecting Patients for Surgery
As the new results demonstrate, liver cancer “is a very treatable” disease for children with hepatoblastoma that can be surgically removed at diagnosis, said Greg Tiao, M.D., a pediatric surgeon at Cincinnati Children’s Hospital and an investigator on the trial.
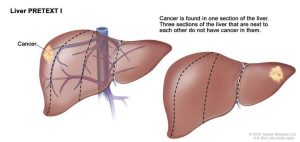
To help doctors identify children with hepatoblastoma who can safely undergo surgery at diagnosis, Rebecka Meyers, M.D., of the University of Utah Hospital and an investigator on the trial, led a team that developed guidelines for identifying tumors that can be removed safely based on imaging studies.
For example, patients with tumors that affect part of the liver, rather than the entire liver, may be candidates for surgery.
These guidelines were incorporated into the clinical trial. Until now, surgeons have relied primarily on their own knowledge and experience to decide which patients were candidates to have their tumors removed.
“But even surgeons at large medical centers who see children with cancer might only see one or two patients with hepatoblastoma each year,” said Dr. Tiao.
Follow-up and larger studies will be needed to determine how the use of the guidelines may influence the selection of patients and patient outcomes, the researchers noted.
An International Trial for Children with Liver Cancer
The approach of using fewer cycles of chemotherapy following surgery for children newly diagnosed with hepatoblastoma is being evaluated further in a large international clinical trial that is under way in North America, Europe, Japan, and Australia.
This study will assess various treatment approaches in approximately 1,200 children.
For example, some patients whose tumors cannot be removed surgically at diagnosis will initially receive chemotherapy to reduce the size of their tumors, potentially making it possible for the tumors to be removed by surgery.
The trial is expected to provide the evidence that will help to establish standard treatments for all patients with hepatoblastoma in the future.
“This is the first trial in hepatoblastoma that’s truly been organized internationally,” said Dr. Katzenstein. “The results will provide the evidence base from a large international study to know when we can safely give patients less chemotherapy and thereby avoid the problems associated with it.”
Source: National Cancer Institute
